Awakening hope: The critical role sleep plays in brain health
How a VCU Parkinson’s and Movement Disorders Center sleep study offers new insights and optimism for patients

Brian Berman, M.D., director of the VCU Parkinson’s and Movement Disorders Center, is investigating the mysteries of neurodegeneration. The evidence he’s discovered points to a surprising culprit: sleep. (Photo by Daniel Sangjib Min, MCV Foundation)
When Ken Konopky was diagnosed with Parkinson's disease at age 54, his life shifted dramatically. What began as minor gait issues soon evolved into tremors, vivid and sometimes violent dreams, and cognitive challenges. By age 61, the former supply chain analyst found himself grappling with both the symptoms of Parkinson's and the uncertainties of living with a progressive neurological disorder.
A self-described heavy sleeper who "hardly ever dreamed," Konopky's concern grew when his dreams blossomed into experiences that caused him to fall out of bed, or think he was climbing out a window or down a ladder. With his expanding set of symptoms also came an equally expansive curiosity to understand his condition.
"I'm not going to sit at home and ask, 'Why me?'" Konopky says. "I'm going to live my life the best I can and find ways to adapt."
That drive brought him to the VCU Parkinson's and Movement Disorders Center, where he found more than a team of physicians — he found a partner in his journey. One opportunity stood out: participation in a sleep study led by Brian Berman, M.D., director of the PMDC and an expert in the intersection of sleep and neurodegeneration. For Konopky, the study offered both insights into his condition and hope for others.
"I've always believed that knowledge is power," Konopky says. "When I see an opportunity to learn more about Parkinson's, I jump at it."
The sleep study: A window into neurodegeneration
The study, which Berman formally launched in 2019 with initial funding from the Parkinson's Foundation, investigates the critical role sleep plays in general brain health, as well as its implications for neurodegenerative diseases like Parkinson's.
At its core, the research being led by Berman and his team aims to unravel a complex cycle experienced by many patients living with Parkinson's: disrupted sleep increases neuroinflammation, leads to memory and other cognitive impairments, and hinders the brain's ability to clear toxins, potentially leading to accelerated neurodegeneration.
Central to the study is the glymphatic system, a network of vessels in the brain responsible for clearing waste, often described as an "oil change" for the mind. Discovered in 2012, the glymphatic system operates most efficiently during deep, uninterrupted sleep.
"Sleep isn't just about rest," explains Berman, a professor in the Department of Neurology. "It's a time when the brain performs critical maintenance. Without good sleep, the risk of neurodegenerative diseases increases."
Combining advanced imaging techniques, blood biomarker analysis and cognitive testing, the study investigates how sleep fragmentation affects brain structure and function, toxin clearance from the brain, and cognitive function in Parkinson's patients compared to healthy control subjects.
For people with Parkinson's, a good night's sleep can feel out of reach. Restless nights filled with vivid dreams, frequent wake-ups and daytime exhaustion are common, while symptoms like stiffness and dream-enacting further disrupt precious rest.
Early findings suggest that differences in biomarkers and toxin clearance are observable after just one night, and that patients with more fragmented sleep show reduced cognitive performance and higher levels of neuroinflammation.
Berman's team has also uncovered significant differences in sleep efficiency and quality between Parkinson's patients and healthy controls. They've documented that non-REM sleep – which is essential for memory storage and retrieval – is disrupted in patients with mild cognitive impairment, a precursor to dementia, more than those patients with normal cognitive function.
Empowering patients through research
For Konopky, participation in the study has been transformative. The experience offered clarity about his condition and underscored the compassionate care he receives at VCU.
"Dr. Berman spends time answering my questions, often with students present," Konopky says. "It's not just about treating me. It's about educating the next generation of doctors, too."
"In my past life as a business analyst, I loved learning and problem-solving," Konopky says. "This study gave me a chance to understand my condition better and feel like I was part of something bigger. It's a positive experience, and it gives me hope."
Konopky has also found ways to bring his generosity of spirit beyond the study. He has spoken on frequent occasions to VCU pharmacy, nursing and physical therapy students, sharing his experiences to help future health care providers understand the human side of Parkinson's.
"It's about making connections," Konopky says, "and showing people that even with this illness, you can live a meaningful life."
A lasting, and widening, legacy
Berman holds the Bemiss Endowed Chair, a philanthropically-funded faculty position named in honor of the late Margaret and Fitzgerald "Gerry" Bemiss. The couple's advocacy and determination to find answers for patients and families were instrumental in both establishing the PMDC and recruiting Berman to VCU.
"Every breakthrough starts with a question," Berman says. "The Bemiss Chair provides me the financial support to both see patients in clinic and explore meaningful research questions with the goal of translating discoveries into better outcomes for patients."
The 2007 gift to establish the chair continues to fuel discovery and collaboration at the PMDC and across VCU. For the sleep study, a clinical research coordinator conducts the imaging and cognitive testing, and the sleep study is completed at the VCU Center for Sleep Medicine (see sidebar).
Experts in the College of Engineering and the School of Public Health work alongside Dr. Berman to provide complex data analysis essential to drawing meaningful and accurate conclusions. Faculty in the School of Nursing also play a crucial role by supporting the team's blood biomarker analysis.
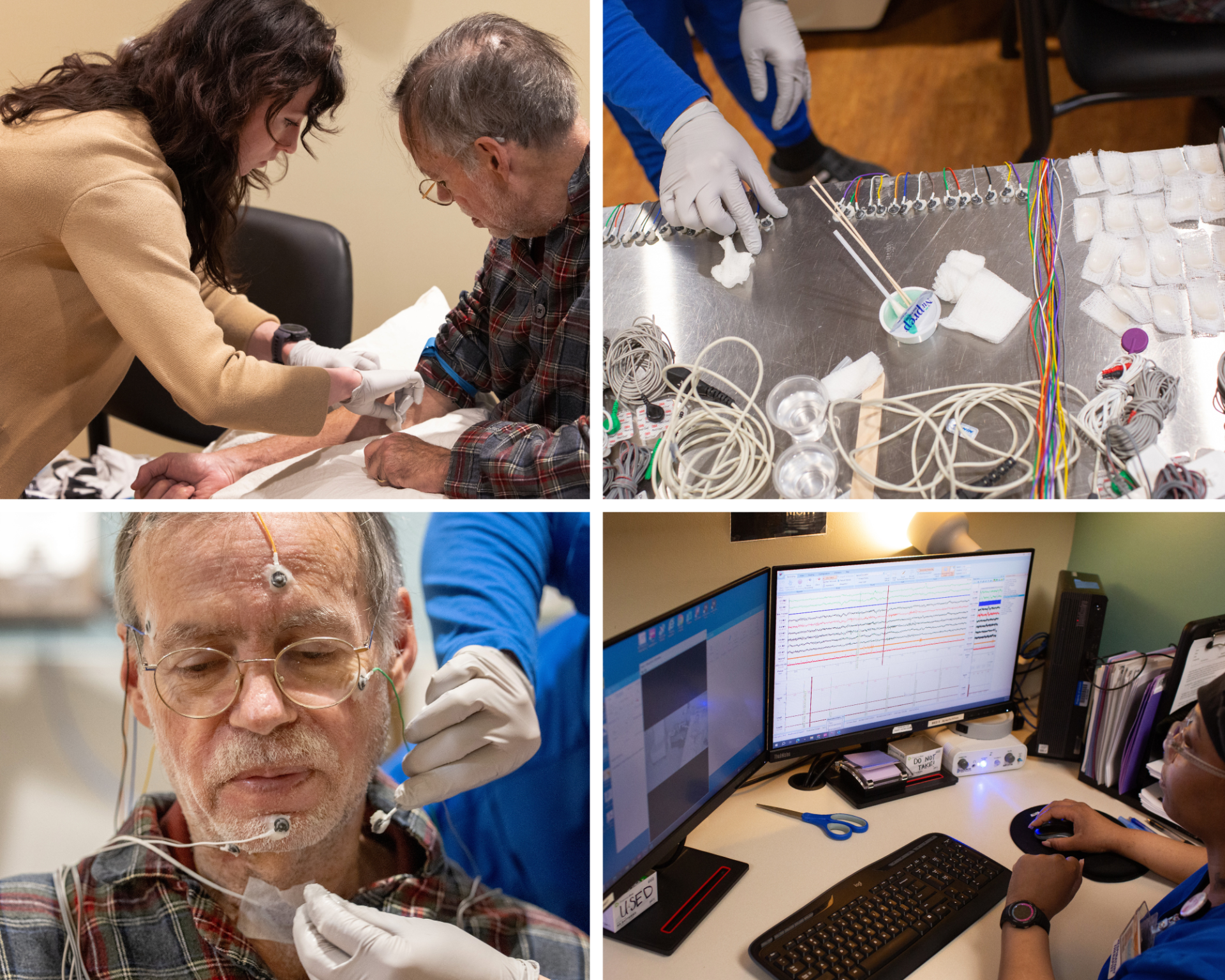
Caileigh Dintino (top left), a clinical research coordinator at the Parkinson's and Movement Disorders Center, readies a patient for his blood draw before his sleep study. According to Berman, Dintino's dedication has been the driving force behind the success of the project. "As researchers, we develop the ideas and designs of studies, but it takes a clinical research coordinator like Caileigh who pours her heart and soul into every detail of the study to ensure that the research is completed and that advances in the field are made," says Berman, who also notes his deep appreciation for the team members at the VCU Center for Sleep Medicine. (Photos by Daniel Sangjib Min, MCV Foundation)
Looking ahead, Berman is interested in developing a longitudinal study to explore how sleep patterns influence cognitive decline, and he sees potential for testing interventions such as neurostimulation during sleep to enhance toxin clearance and possibly slow neurodegeneration. Another promising avenue is the development of home-based sleep monitoring technologies, which could make the research more accessible to a wider range of participants.
While the study's immediate goal is to understand the link between sleep and neurodegeneration, its long-term potential excites Konopky.
"VCU has given me incredible care and the opportunity to learn," Konopky says. "I'm grateful to be part of something that's changing lives, and I'm optimistic about what's ahead."
To learn more about supporting the VCU Parkinson's and Movement Disorders Center, contact Bernadette O'Shea, senior director of development, at osheab@vcu.edu.
To learn more about the sleep study discussed in this story, contact Caileigh Dintino, clinical research coordinator, at caileigh.dintino@vcuhealth.org.
When Ken Konopky was diagnosed with Parkinson's disease at age 54, his life shifted dramatically. What began as minor gait issues soon evolved into tremors, vivid and sometimes violent dreams, and cognitive challenges. By age 61, the former supply chain analyst found himself grappling with both the symptoms of Parkinson's and the uncertainties of living with a progressive neurological disorder.
A self-described heavy sleeper who "hardly ever dreamed," Konopky's concern grew when his dreams blossomed into experiences that caused him to fall out of bed, or think he was climbing out a window or down a ladder. With his expanding set of symptoms also came an equally expansive curiosity to understand his condition.
"I'm not going to sit at home and ask, 'Why me?'" Konopky says. "I'm going to live my life the best I can and find ways to adapt."
That drive brought him to the VCU Parkinson's and Movement Disorders Center, where he found more than a team of physicians — he found a partner in his journey. One opportunity stood out: participation in a sleep study led by Brian Berman, M.D., director of the PMDC and an expert in the intersection of sleep and neurodegeneration. For Konopky, the study offered both insights into his condition and hope for others.
"I've always believed that knowledge is power," Konopky says. "When I see an opportunity to learn more about Parkinson's, I jump at it."
The sleep study: A window into neurodegeneration
The study, which Berman formally launched in 2019 with initial funding from the Parkinson's Foundation, investigates the critical role sleep plays in general brain health, as well as its implications for neurodegenerative diseases like Parkinson's.
At its core, the research being led by Berman and his team aims to unravel a complex cycle experienced by many patients living with Parkinson's: disrupted sleep increases neuroinflammation, leads to memory and other cognitive impairments, and hinders the brain's ability to clear toxins, potentially leading to accelerated neurodegeneration.
Central to the study is the glymphatic system, a network of vessels in the brain responsible for clearing waste, often described as an "oil change" for the mind. Discovered in 2012, the glymphatic system operates most efficiently during deep, uninterrupted sleep.
"Sleep isn't just about rest," explains Berman, a professor in the Department of Neurology. "It's a time when the brain performs critical maintenance. Without good sleep, the risk of neurodegenerative diseases increases."
Combining advanced imaging techniques, blood biomarker analysis and cognitive testing, the study investigates how sleep fragmentation affects brain structure and function, toxin clearance from the brain, and cognitive function in Parkinson's patients compared to healthy control subjects.
For people with Parkinson's, a good night's sleep can feel out of reach. Restless nights filled with vivid dreams, frequent wake-ups and daytime exhaustion are common, while symptoms like stiffness and dream-enacting further disrupt precious rest.
Early findings suggest that differences in biomarkers and toxin clearance are observable after just one night, and that patients with more fragmented sleep show reduced cognitive performance and higher levels of neuroinflammation.
Berman's team has also uncovered significant differences in sleep efficiency and quality between Parkinson's patients and healthy controls. They've documented that non-REM sleep – which is essential for memory storage and retrieval – is disrupted in patients with mild cognitive impairment, a precursor to dementia, more than those patients with normal cognitive function.
Empowering patients through research
For Konopky, participation in the study has been transformative. The experience offered clarity about his condition and underscored the compassionate care he receives at VCU.
"Dr. Berman spends time answering my questions, often with students present," Konopky says. "It's not just about treating me. It's about educating the next generation of doctors, too."
"In my past life as a business analyst, I loved learning and problem-solving," Konopky says. "This study gave me a chance to understand my condition better and feel like I was part of something bigger. It's a positive experience, and it gives me hope."
Konopky has also found ways to bring his generosity of spirit beyond the study. He has spoken on frequent occasions to VCU pharmacy, nursing and physical therapy students, sharing his experiences to help future health care providers understand the human side of Parkinson's.
"It's about making connections," Konopky says, "and showing people that even with this illness, you can live a meaningful life."
A lasting, and widening, legacy
Berman holds the Bemiss Endowed Chair, a philanthropically-funded faculty position named in honor of the late Margaret and Fitzgerald "Gerry" Bemiss. The couple's advocacy and determination to find answers for patients and families were instrumental in both establishing the PMDC and recruiting Berman to VCU.
"Every breakthrough starts with a question," Berman says. "The Bemiss Chair provides me the financial support to both see patients in clinic and explore meaningful research questions with the goal of translating discoveries into better outcomes for patients."
The 2007 gift to establish the chair continues to fuel discovery and collaboration at the PMDC and across VCU. For the sleep study, a clinical research coordinator conducts the imaging and cognitive testing, and the sleep study is completed at the VCU Center for Sleep Medicine (see sidebar).
Experts in the College of Engineering and the School of Public Health work alongside Dr. Berman to provide complex data analysis essential to drawing meaningful and accurate conclusions. Faculty in the School of Nursing also play a crucial role by supporting the team's blood biomarker analysis.
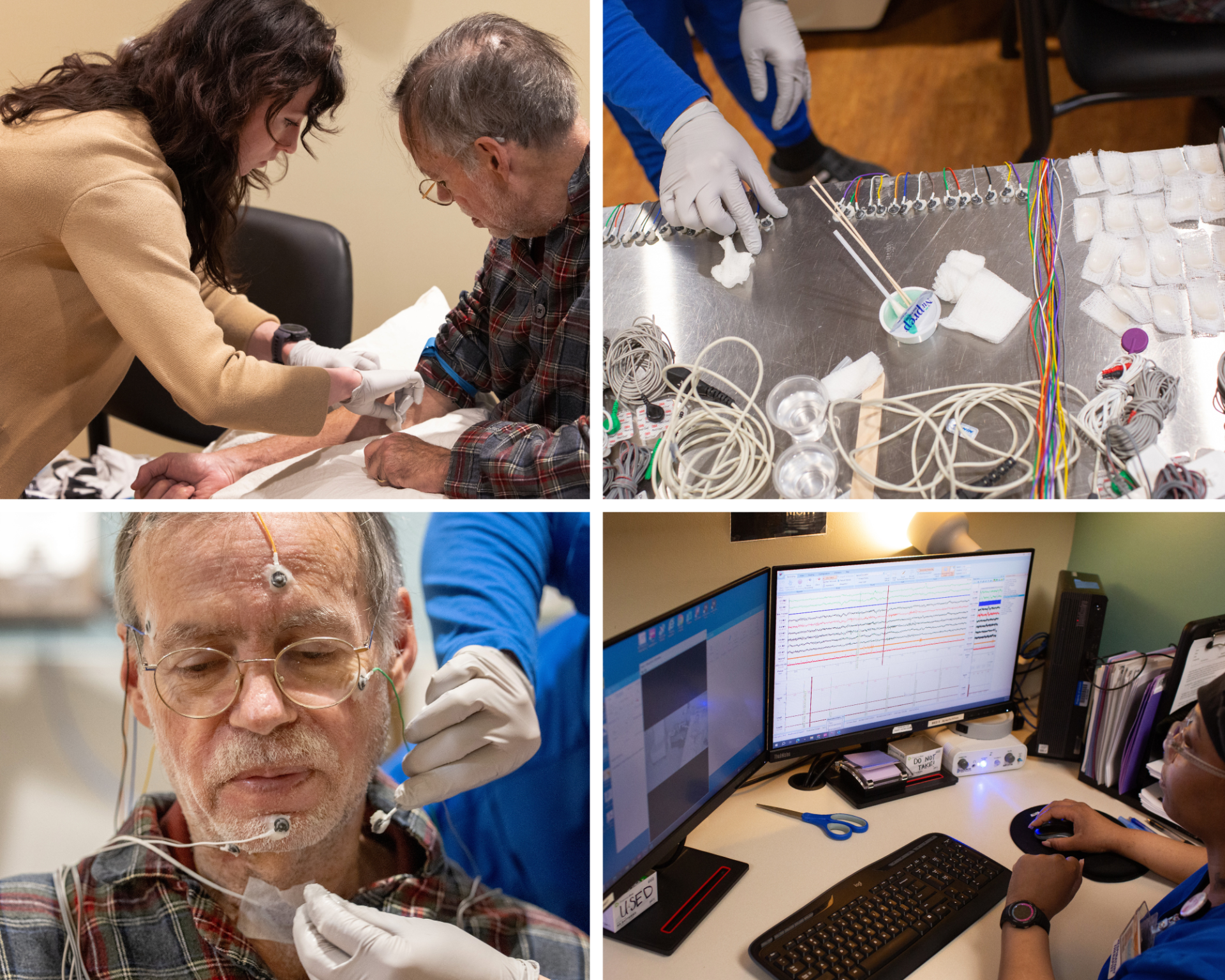
Caileigh Dintino (top left), a clinical research coordinator at the Parkinson's and Movement Disorders Center, readies a patient for his blood draw before his sleep study. According to Berman, Dintino's dedication has been the driving force behind the success of the project. "As researchers, we develop the ideas and designs of studies, but it takes a clinical research coordinator like Caileigh who pours her heart and soul into every detail of the study to ensure that the research is completed and that advances in the field are made," says Berman, who also notes his deep appreciation for the team members at the VCU Center for Sleep Medicine. (Photos by Daniel Sangjib Min, MCV Foundation)
Looking ahead, Berman is interested in developing a longitudinal study to explore how sleep patterns influence cognitive decline, and he sees potential for testing interventions such as neurostimulation during sleep to enhance toxin clearance and possibly slow neurodegeneration. Another promising avenue is the development of home-based sleep monitoring technologies, which could make the research more accessible to a wider range of participants.
While the study's immediate goal is to understand the link between sleep and neurodegeneration, its long-term potential excites Konopky.
"VCU has given me incredible care and the opportunity to learn," Konopky says. "I'm grateful to be part of something that's changing lives, and I'm optimistic about what's ahead."
To learn more about supporting the VCU Parkinson's and Movement Disorders Center, contact Bernadette O'Shea, senior director of development, at osheab@vcu.edu.
To learn more about the sleep study discussed in this story, contact Caileigh Dintino, clinical research coordinator, at caileigh.dintino@vcuhealth.org.
Center for Sleep Medicine
The VCU Health Center for Sleep Medicine is the longest-operating sleep clinic in the Richmond, Virginia, area, and serves both adult and pediatric patients.
Under the leadership of sleep specialist Maha Alattar, M.D., the center addresses the full spectrum of sleep disorders, from common conditions like insomnia and sleep apnea to the most complex cases. Patients benefit from a range of diagnostic options, including overnight, daytime and at-home sleep studies.
Combining advanced technology, interdisciplinary collaboration and personalized care, the center leads the way in improving sleep health and quality of life for the Richmond community.
Tags: