From stress pathways to life-saving drones, VCU Health researchers plot a new course toward improved heart health
How team science and novel thinking are pushing boundaries in cardiovascular medicine

Innovative research underway at VCU Health aims to reshape the landscape of heart disease treatment.
At the heart of VCU Health’s mission lies a commitment to groundbreaking research, community engagement and patient-centered care. Now, two trailblazing research projects funded by the American Heart Association are bridging the gaps for patients who face the life-threatening challenges of cardiovascular disease. Together, these efforts aim to improve access to care, reduce disparities and enhance outcomes for patients, whether they face the daily toll of chronic stress or the sudden peril of cardiac arrest.
Mapping chronic stress to prevent cardiovascular disease
Thanks to a $15 million grant from the AHA’s Strategically Focused Research Network program, VCU Health’s Pauley Heart Center is investigating the molecular underpinnings of how chronic stress impacts cardiovascular health. This study – the first of its kind at VCU – seeks to uncover the physiological effects of prolonged periods of stress and develop effective, real-world solutions for vulnerable populations.
“Stress isn’t just a mental burden,” explains W. Gregory Hundley, M’88, Pauley director. “It’s also a physiological one.”
The AHA SFRN research project integrates expertise from Pauley and the School of Medicine’s departments of Psychiatry and Internal Medicine, as well as the Department of Kinesiology and Health Sciences in the College of Humanities and Sciences. Together, the team is investigating how different diet and exercise plans might serve as a treatment for stress-induced cardiovascular damage, particularly in cancer patients.
"We’re studying what happens at the cellular level, how inflammation is triggered and how stress impacts brain activity, which in turn affects the heart," Hundley says. "This team science approach allows us to explore these interactions in unprecedented detail."
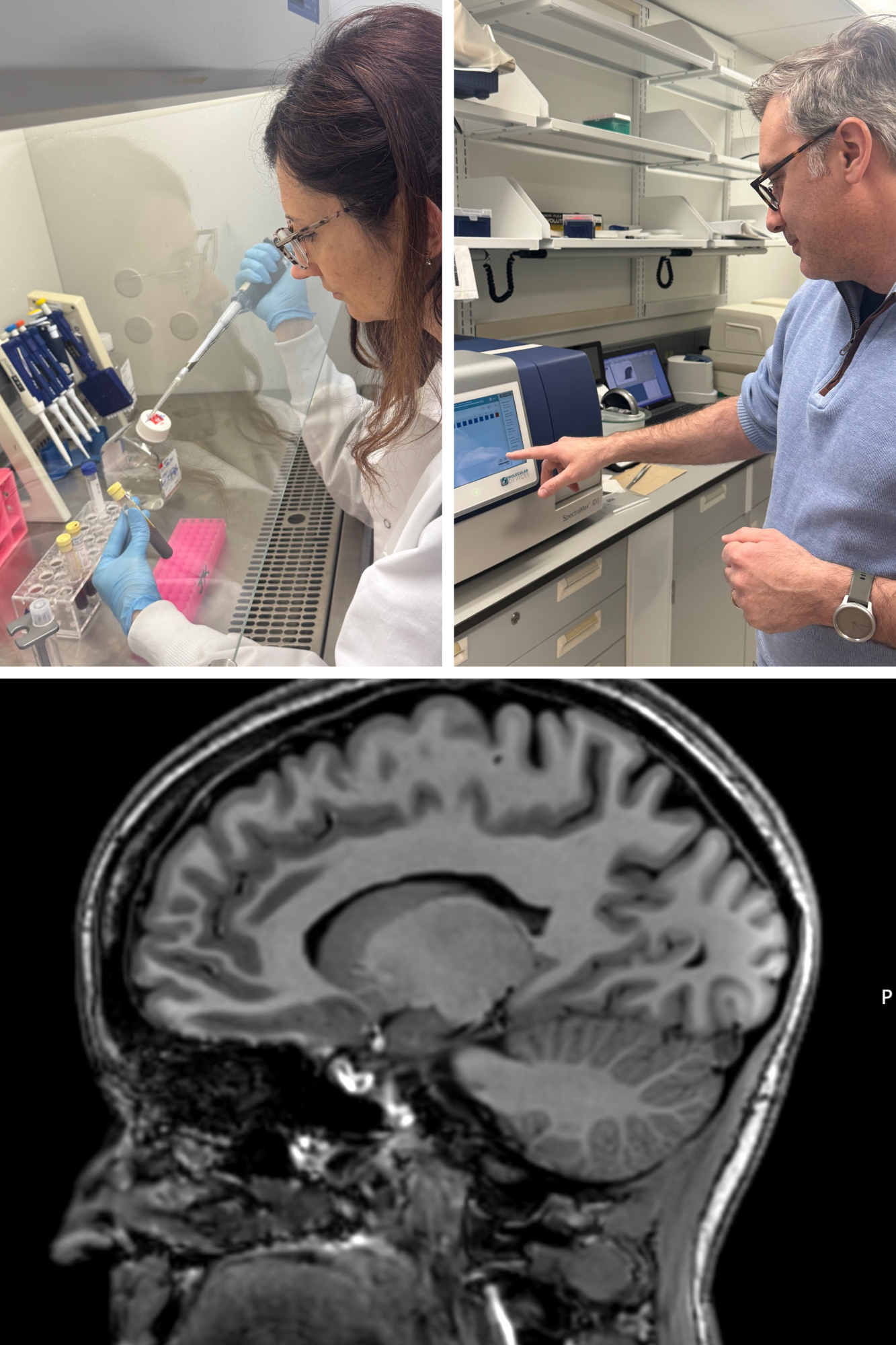
Eleonora Mezzaroma, Ph.D., and Adolfo Mauro, Ph.D., are investigators at Pauley Heart Center studying the impact of prolonged periods of stress on cardiovascular health. By delving into the brain’s role as an intermediary in the body’s stress response – commonly called the fight-or-flight system – imaging helps the team see how stress-induced brain activation leads to systemic inflammation and heart disease (Photos courtesy of Pauley Heart Center).
A few members of the research team are also supported by endowed chairs. Made possible by private gifts from donors, these endowed funds play a pivotal role in providing the top scientists on the MCV Campus with the necessary resources to pursue ambitious research projects. For example, in Pauley, Hundley holds the George W. Vetrovec Chair in the Division of Cardiology while Salloum holds the Natalie N. and John R. Congdon Sr. Endowed Chair. Similarly, Moeller holds the C. Kenneth and Dianne Wright Distinguished Chair in Clinical and Translational Research.
“Scientific research is very time- and resource-intensive,” Hundley explains. “Endowed positions allow us to advance the field of cardiovascular medicine and maybe even help change the human condition in some measurable way. Without these important positions, most faculty members would only be able to either practice or teach, meaning the field would advance at a slower pace.”
Revolutionizing emergency cardiac care with drone technology
Meanwhile, a technological revolution is taking flight in James City County, Virginia. A pioneering project will be testing drones as a faster means of delivering automated external defibrillators to bystanders so they can treat out-of-hospital cardiac arrest victims before first responders can get to the scene. Led by Emergency Medicine’s Joseph P. Ornato, M.D., and supported by a four-year, $4 million AHA grant, the initiative aims to reduce the time to get the heart started again and improve survival rates.
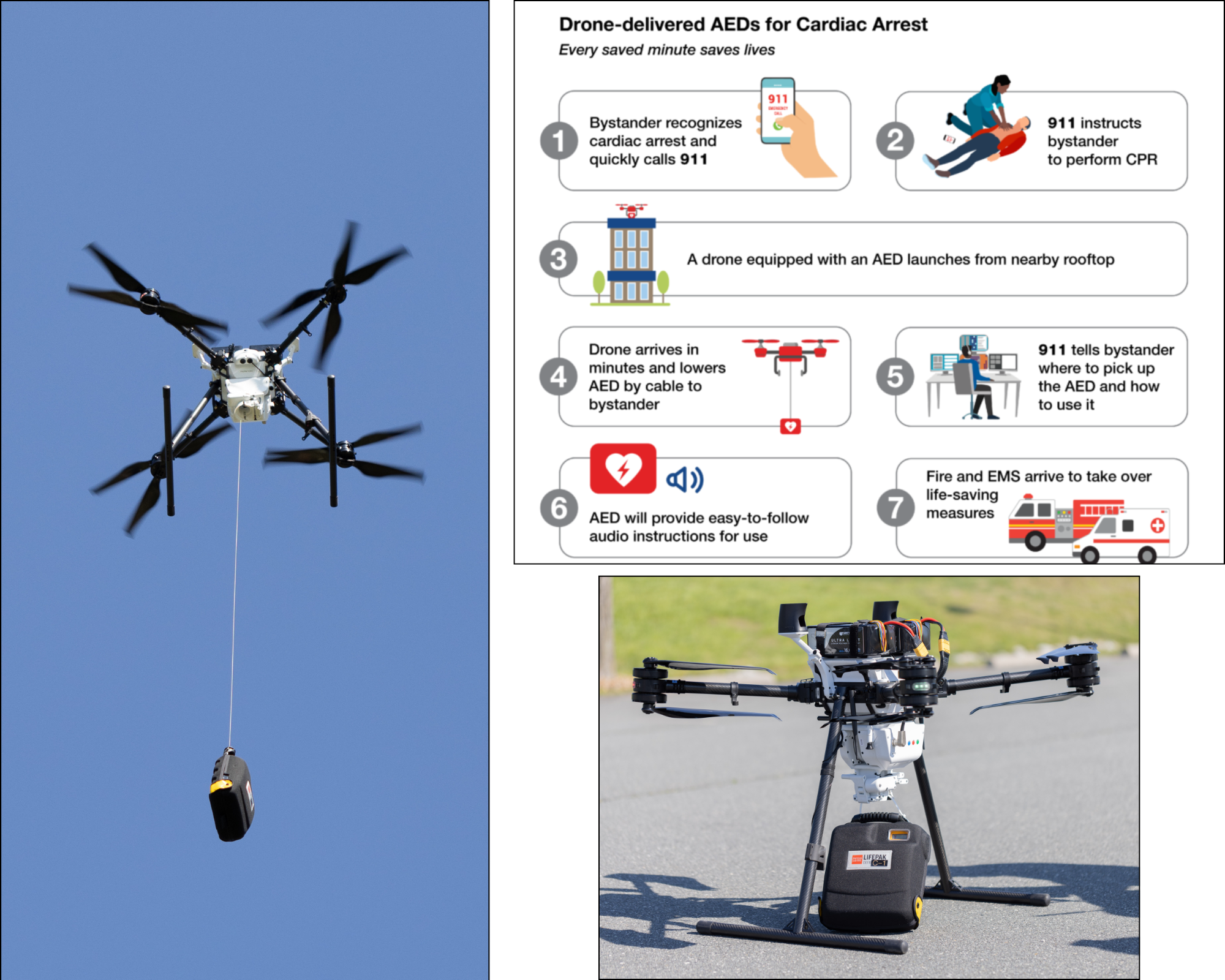
After calling 911, bystanders will receive step-by-step instructions for performing CPR and using the AED until first responders arrive (Photos courtesy of Forsyth County, NC Sheriff’s Office).
Every year, more than 350,000 Americans experience sudden cardiac arrest, with survival chances dropping 10% with each minute of delay to treatment. If defibrillation occurs within the first minute, survival rates are as high as 90%. However, traditional emergency medical services responders often take 8 to 10 minutes to reach a patient and several more minutes before they can attach their equipment and, if indicated, deliver a defibrillation shock to restart the heart.
“The enemy is time to initial treatment,” Ornato explains. “The effectiveness of rapid treatment is high, and although our emergency care providers are well trained, the critical issue is how long it takes to reach the patient.”
Nearly a decade ago, Ornato secured a National Institutes of Health grant to explore drone delivery of lifesaving treatments, such as naloxone for opioid overdoses and AEDs for cardiac arrest. His team trained Richmond’s 911 medical dispatchers as Federal Aviation Administration-certified drone pilots, equipping them with the skills to operate drones in emergencies. In a simulation study, dispatchers guided bystanders through a mock fentanyl overdose, instructing them to retrieve naloxone from a landed drone and administer it to a manikin. Every participant completed the task in an average of 2 minutes and 2 seconds after 911 call receipt, demonstrating the potential for drones to accelerate critical interventions.
Ornato, an experienced physician-scientist and instrument-rated jet and drone pilot, has a long history of innovation. More than two decades ago, he and his wife, cardiologist Mary Ann Peberdy, M.D., led a clinical trial that secured FDA approval for public access to AEDs. This breakthrough made AEDs widely available in public spaces, saving an estimated 10,000 lives in the United States each year. Building on that legacy, Ornato saw an opportunity to harness advances in drone technology to improve the life-or-death urgency of cardiac arrest care.
“During the naloxone trial, I noticed that some of the new drones coming on the market were larger, faster and safer,” Ornato recalls. “I thought, ‘What if we could use them to deliver AEDs?’”
That’s when Bob and Margaret Hershberger of Williamsburg, Virginia, stepped in to fund a feasibility study demonstrating the concept’s viability. The couple has a deeply personal connection to cardiovascular research – Bob suffered a cardiac arrest while exercising, and Peberdy saved his life.
“The Hershbergers are hero public citizens,” Ornato says. “Without their support, we’d have nothing more than a dream in our heads.”
Based on their support, the VCU team was able to press forward and demonstrate the potential of drone-delivered AEDs – a development that positioned them to collaborate with a colleague at Duke University. Together, they secured the current AHA grant at the pivotal moment when new FAA regulations were finally making such a strategy legally feasible, an option that wasn't available when the VCU team was prepared to launch a pilot trial of drone-delivered naloxone a decade prior.
As part of the AHA grant, the team was required to launch the project in less densely populated areas, where innovative solutions could help bridge gaps in emergency care. Each site needed an established law enforcement drone program with experienced pilots already conducting tactical and surveillance missions. The Duke team selected Forsyth County, North Carolina, while the VCU team chose James City County, just outside Williamsburg.
Now, 18 months into the project, both sites have secured the necessary FAA certifications, and AED drone deliveries are set to begin within months – nearly a year ahead of schedule. The lessons learned from this initiative will serve as a model for expanding FAA-approved drone-delivered AED services nationwide, helping more cardiac arrest victims receive lifesaving care when every second counts.
A unified vision for better cardiovascular care
From exploring the molecular impacts of stress to deploying leading-edge drone technology, VCU Health is advancing innovative solutions to today’s most pressing cardiovascular challenges. Both initiatives exemplify the power of collaboration, philanthropy and patient-centered research.
“Our strength lies in our ability to bring together experts across disciplines to tackle big questions,” Hundley says. “With the trust of our community and the support of visionary donors, we are paving the way for a healthier future.”
If you would like to support cardiovascular research contact Justin Jannuzzi, senior director of development, at jannuzzijp@vcu.edu.
At the heart of VCU Health’s mission lies a commitment to groundbreaking research, community engagement and patient-centered care. Now, two trailblazing research projects funded by the American Heart Association are bridging the gaps for patients who face the life-threatening challenges of cardiovascular disease. Together, these efforts aim to improve access to care, reduce disparities and enhance outcomes for patients, whether they face the daily toll of chronic stress or the sudden peril of cardiac arrest.
Mapping chronic stress to prevent cardiovascular disease
Thanks to a $15 million grant from the AHA’s Strategically Focused Research Network program, VCU Health’s Pauley Heart Center is investigating the molecular underpinnings of how chronic stress impacts cardiovascular health. This study – the first of its kind at VCU – seeks to uncover the physiological effects of prolonged periods of stress and develop effective, real-world solutions for vulnerable populations.
“Stress isn’t just a mental burden,” explains W. Gregory Hundley, M’88, Pauley director. “It’s also a physiological one.”
The AHA SFRN research project integrates expertise from Pauley and the School of Medicine’s departments of Psychiatry and Internal Medicine, as well as the Department of Kinesiology and Health Sciences in the College of Humanities and Sciences. Together, the team is investigating how different diet and exercise plans might serve as a treatment for stress-induced cardiovascular damage, particularly in cancer patients.
"We’re studying what happens at the cellular level, how inflammation is triggered and how stress impacts brain activity, which in turn affects the heart," Hundley says. "This team science approach allows us to explore these interactions in unprecedented detail."
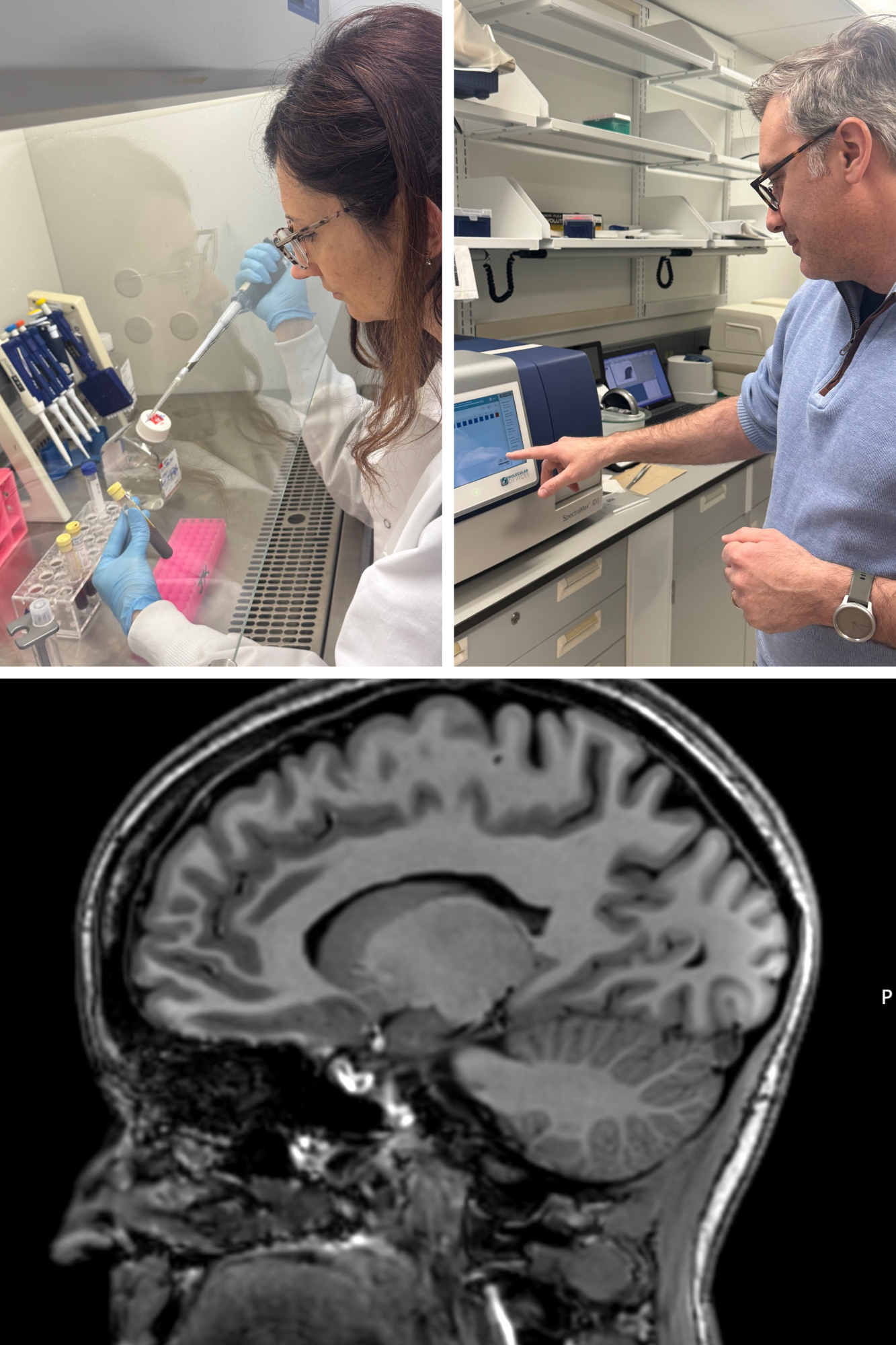
Eleonora Mezzaroma, Ph.D., and Adolfo Mauro, Ph.D., are investigators at Pauley Heart Center studying the impact of prolonged periods of stress on cardiovascular health. By delving into the brain’s role as an intermediary in the body’s stress response – commonly called the fight-or-flight system – imaging helps the team see how stress-induced brain activation leads to systemic inflammation and heart disease (Photos courtesy of Pauley Heart Center).
A few members of the research team are also supported by endowed chairs. Made possible by private gifts from donors, these endowed funds play a pivotal role in providing the top scientists on the MCV Campus with the necessary resources to pursue ambitious research projects. For example, in Pauley, Hundley holds the George W. Vetrovec Chair in the Division of Cardiology while Salloum holds the Natalie N. and John R. Congdon Sr. Endowed Chair. Similarly, Moeller holds the C. Kenneth and Dianne Wright Distinguished Chair in Clinical and Translational Research.
“Scientific research is very time- and resource-intensive,” Hundley explains. “Endowed positions allow us to advance the field of cardiovascular medicine and maybe even help change the human condition in some measurable way. Without these important positions, most faculty members would only be able to either practice or teach, meaning the field would advance at a slower pace.”
Revolutionizing emergency cardiac care with drone technology
Meanwhile, a technological revolution is taking flight in James City County, Virginia. A pioneering project will be testing drones as a faster means of delivering automated external defibrillators to bystanders so they can treat out-of-hospital cardiac arrest victims before first responders can get to the scene. Led by Emergency Medicine’s Joseph P. Ornato, M.D., and supported by a four-year, $4 million AHA grant, the initiative aims to reduce the time to get the heart started again and improve survival rates.
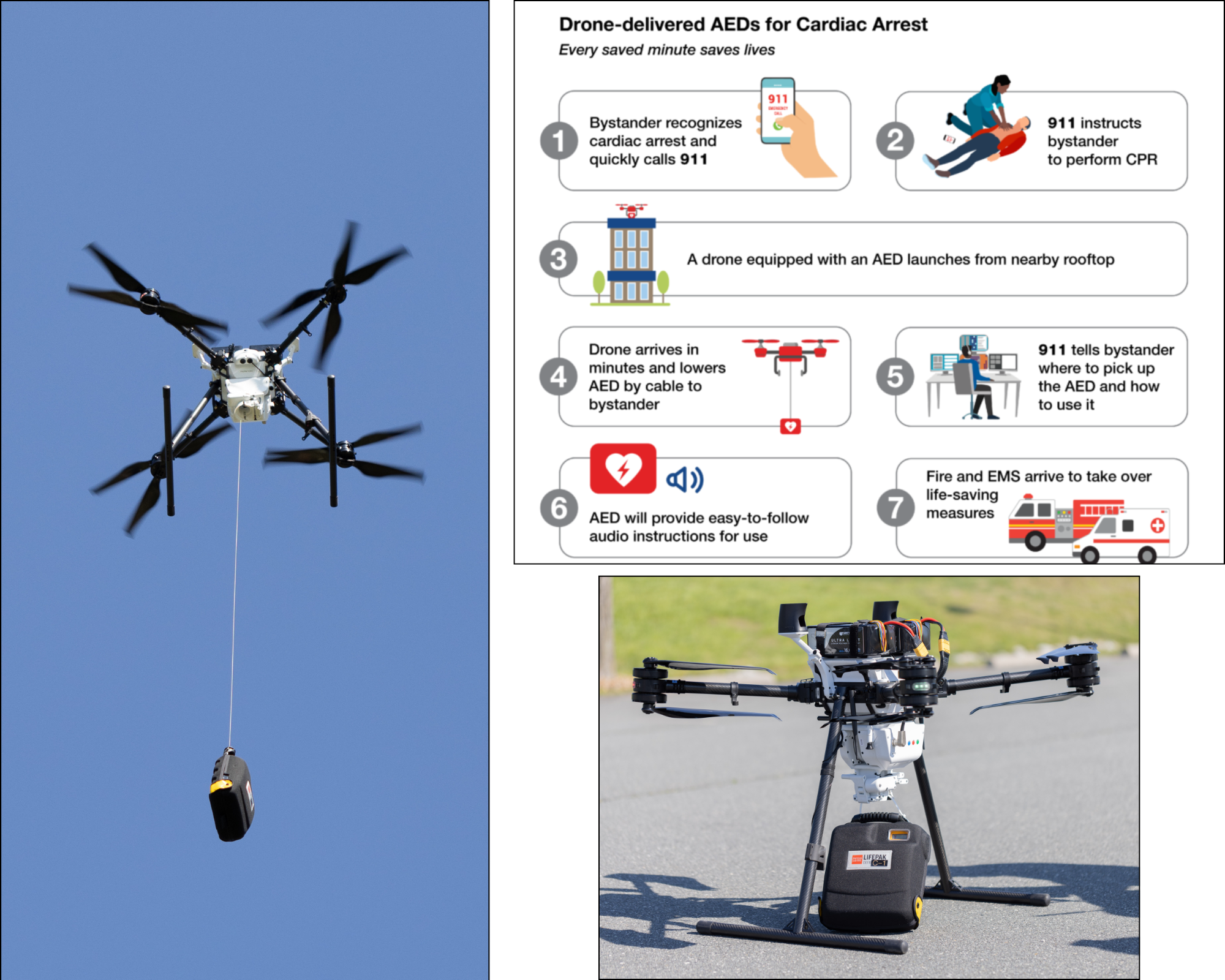
After calling 911, bystanders will receive step-by-step instructions for performing CPR and using the AED until first responders arrive (Photos courtesy of Forsyth County, NC Sheriff’s Office).
Every year, more than 350,000 Americans experience sudden cardiac arrest, with survival chances dropping 10% with each minute of delay to treatment. If defibrillation occurs within the first minute, survival rates are as high as 90%. However, traditional emergency medical services responders often take 8 to 10 minutes to reach a patient and several more minutes before they can attach their equipment and, if indicated, deliver a defibrillation shock to restart the heart.
“The enemy is time to initial treatment,” Ornato explains. “The effectiveness of rapid treatment is high, and although our emergency care providers are well trained, the critical issue is how long it takes to reach the patient.”
Nearly a decade ago, Ornato secured a National Institutes of Health grant to explore drone delivery of lifesaving treatments, such as naloxone for opioid overdoses and AEDs for cardiac arrest. His team trained Richmond’s 911 medical dispatchers as Federal Aviation Administration-certified drone pilots, equipping them with the skills to operate drones in emergencies. In a simulation study, dispatchers guided bystanders through a mock fentanyl overdose, instructing them to retrieve naloxone from a landed drone and administer it to a manikin. Every participant completed the task in an average of 2 minutes and 2 seconds after 911 call receipt, demonstrating the potential for drones to accelerate critical interventions.
Ornato, an experienced physician-scientist and instrument-rated jet and drone pilot, has a long history of innovation. More than two decades ago, he and his wife, cardiologist Mary Ann Peberdy, M.D., led a clinical trial that secured FDA approval for public access to AEDs. This breakthrough made AEDs widely available in public spaces, saving an estimated 10,000 lives in the United States each year. Building on that legacy, Ornato saw an opportunity to harness advances in drone technology to improve the life-or-death urgency of cardiac arrest care.
“During the naloxone trial, I noticed that some of the new drones coming on the market were larger, faster and safer,” Ornato recalls. “I thought, ‘What if we could use them to deliver AEDs?’”
That’s when Bob and Margaret Hershberger of Williamsburg, Virginia, stepped in to fund a feasibility study demonstrating the concept’s viability. The couple has a deeply personal connection to cardiovascular research – Bob suffered a cardiac arrest while exercising, and Peberdy saved his life.
“The Hershbergers are hero public citizens,” Ornato says. “Without their support, we’d have nothing more than a dream in our heads.”
Based on their support, the VCU team was able to press forward and demonstrate the potential of drone-delivered AEDs – a development that positioned them to collaborate with a colleague at Duke University. Together, they secured the current AHA grant at the pivotal moment when new FAA regulations were finally making such a strategy legally feasible, an option that wasn't available when the VCU team was prepared to launch a pilot trial of drone-delivered naloxone a decade prior.
As part of the AHA grant, the team was required to launch the project in less densely populated areas, where innovative solutions could help bridge gaps in emergency care. Each site needed an established law enforcement drone program with experienced pilots already conducting tactical and surveillance missions. The Duke team selected Forsyth County, North Carolina, while the VCU team chose James City County, just outside Williamsburg.
Now, 18 months into the project, both sites have secured the necessary FAA certifications, and AED drone deliveries are set to begin within months – nearly a year ahead of schedule. The lessons learned from this initiative will serve as a model for expanding FAA-approved drone-delivered AED services nationwide, helping more cardiac arrest victims receive lifesaving care when every second counts.
A unified vision for better cardiovascular care
From exploring the molecular impacts of stress to deploying leading-edge drone technology, VCU Health is advancing innovative solutions to today’s most pressing cardiovascular challenges. Both initiatives exemplify the power of collaboration, philanthropy and patient-centered research.
“Our strength lies in our ability to bring together experts across disciplines to tackle big questions,” Hundley says. “With the trust of our community and the support of visionary donors, we are paving the way for a healthier future.”
If you would like to support cardiovascular research contact Justin Jannuzzi, senior director of development, at jannuzzijp@vcu.edu.
Multi-site, multi-disciplinary
Pauley’s research aligns with other AHA SFRN-funded studies at The Ohio State University and the University of California Davis. While VCU explores cellular and behavioral interventions, Ohio State examines the role of health disparities in stress outcomes, and UC Davis investigates molecular pathways linking stress to cardiovascular disease in patients from underserved populations.
Leading key elements of Pauley’s research are VCU-based investigators:
- Psychiatry professor and Wright Center for Clinical and Translational Research Director F. Gerard Moeller, M.D., brings to the team expertise in brain imaging, allowing researchers to map how different stressors influence brain activity and, by extension, cardiovascular health.
- Fadi N. Salloum, PHD’05 (PHIS), associate chair for research in the Department of Internal Medicine, leads efforts to understand cellular responses to stress and develop targeted interventions. Persistent, ongoing bouts of stress can activate inflammatory pathways in the body, damage cells and lead to conditions like heart attacks and strokes.
- A critical component of the research is the behavioral element led by Arnethea Sutton, Ph.D., assistant professor in kinesiology and health sciences, who collaborates with community advisory boards to address barriers to accessing care – ultimately enabling investigators to explore how physical activity can buffer against stress-related damage.
Tags: