Take good care
Scott M. Strayer, M’94, H’97, is a champion — and an exemplar — of the breadth of practice available to family medicine physicians.
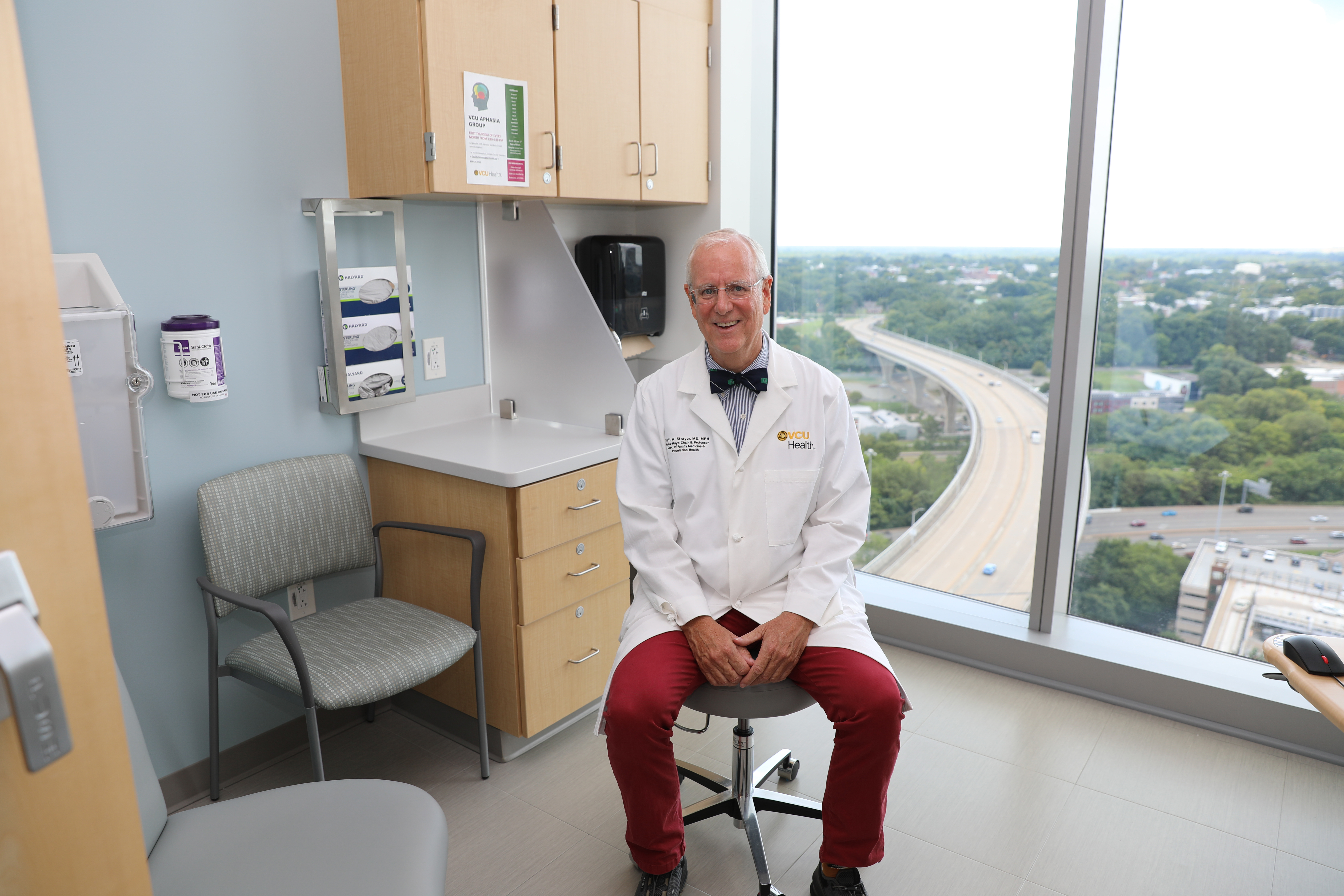
VCU Department of Family Medicine and Population Health Chair Scott M. Strayer, M’94, H’97, sits in the VCU Health Adult Outpatient Pavilion, where larger clinical spaces allowed for the department’s expansion after a move from Nelson Family Medicine in 2023. (Photo by Arda Athman)
Growing up in Southeast Asia and Latin America, Scott M. Strayer, M’94, H’97, developed a worldview that still guides his life.
“My first memories are being raised in Thailand by people who helped my mom nurture and care for us,” he said. The family moved to Peru and traveled extensively in Latin America and Southeast Asia while overseas. Those multicultural experiences led to his interest in medicine and a desire to take care of people.
“Having an open-minded view of people from various backgrounds has really been incredibly important in my life,” he said. “I’m so thankful that I had that upbringing.”
His father’s job led the family from Peru to Chicago then to Abbott Laboratories in Canada where the elder Strayer worked with infant and adult nutritional products. While that journey exposed young Strayer, as he puts it, “to a little bit of a pharmaceutical and food manufacturing background,” it was a later teenage experience that set the stage for his future in family medicine.
“I like to say that I discovered family medicine twice,” he explained. “Our family physician in Canada would spend every bit of one hour for a visit once or twice a year. Out of that hour, 40 or 50 minutes were spent talking. It was amazing how much he was able to draw out in terms of social history, how we were doing in school, career goals and being able to influence in a gentle way. It was a big part of what really attracted me to family medicine.”
While others may be drawn to the field because of a personal medical experience, Strayer is thankful he had no major medical issues.
“My interest was more in the biopsychosocial model and how you can be a positive influence in a teenager’s world,” he said. “Honestly, I thought, ‘Well, that’s what doctors do.’”
He discovered family medicine the second time as a medical student on the MCV Campus.
“I loved everything about every rotation,” he remembered. “I think that’s a typical family doctor story. And I particularly like procedures. I was leaning toward a surgical specialty or subspecialty, but I started to think about what drew me into medicine and about that early teenage influence of my family physician.”
Today, as the Harris-Mayo Chair of the Department of Family Medicine and Population Health, Strayer draws upon those early experiences to help shape his current role as leader, mentor, counselor and educator for future generations of family practitioners.
A catalyst for improved quality of care
When he learned early in his career that Samuel M. Jones, M’79, former program director of the Fairfax Family Medicine Residency, was credentialed in tympanostomy and tonsillectomies for many years, Strayer was intrigued.
“Sam was still surgically placing ear tubes well into his career as a family physician,” he said. “It gave me the idea that if you were really interested in a particular procedure, you could get that additional training and expertise. And, depending upon where you were practicing – if there’s a need for your expertise – you could do that.”
Obstetrics is another example of the far-reaching benefit of advanced training. While it’s not unusual for family physicians to see OB-GYN patients, many go on to become trained in surgical obstetrics procedures not only because of their procedural interest, but also to improve maternal outcomes, particularly in rural areas where patients may have less access to specialists.
Strayer’s own interests in diagnostic procedures, in fact, led to additional training.
“I actually did a deep dive into endoscopy and became proficient and credentialed,” he said. “I’ve been doing that for 20-plus years and helping to train family docs who then go into underserved areas where there is no one to do an endoscopy. Essentially, we are saving people’s lives by providing access to this critical service for cancer screening.”
When more family physicians are in a geographic area, Strayer said, there’s less maternal and cancer morbidity, and mortality — and improved quality of life.
In July, the department welcomed its inaugural cohort to the VCU Health Community Memorial Hospital residency program in South Hill, Virginia. Near the North Carolina border, the residency program helps attract practitioners to a region with one of the highest rates of colon cancer disparities in the country. “Our new family medicine residency in South Hill is going to be a major catalyst for improving health outcomes in that part of the state,” Strayer said.
A living, breathing example
A prolific researcher (see sidebar), Strayer already has plans to “figure out what’s going on” in the 26 counties east of South Hill with one of the highest colorectal cancer death rates in the country.
In this part of the state, many residents may not be getting screened for colorectal cancer at all. For those that do, a positive stool-blood screening result could mean over an hour’s worth of travel for an endoscopy — a distance that Strayer suspects presents additional barriers for residents, such as taking time off work for further testing and follow-up care.
“If we can find some of the causes and some of the treatment interventions, that’s great,” he said, “but at the end of the day, you need to have folks who can help screen patients to identify the disease early and take care of it before it kills you.”
Strayer is dedicated to ensuring that there are enough physicians to take care of screening and follow up to make up for the lack of access to specialists in the region. The new family medicine residency lays the groundwork to make that promise a reality.
That drive to “figure things out” also served him well in medical school.
In his fourth year, he and a fellow student spent the summer working on an olfactory project led by Richard M. Costanzo, Ph.D., now a professor emeritus in the Department of Physiology and Biophysics.
“We had an interesting finding that there might be some smell distortion with the use of a certain antihypertensive,” Strayer remembered. “We presented it at a regional ear, nose and throat conference. It was my first major medical research presentation.”
After Strayer returned as department chair in 2020, Costanzo, who retired in 2018, ran into him at an event on campus.
“It was exciting to see a former student who had advanced his career to this point,” Costanzo said. “It’s such an asset for medicine to have faculty like Scott who have mastered the art of teaching, research and patient care.”
As a resident, Strayer was the primary author on an orthopaedic research article published in American Family Physician. Under the tutelage of Michael J. Petrizzi, M.D., former director of the VCU Hanover Family Practice Residency, Strayer and fellow resident Steven G. Reece, M’94, H’97, studied treatments and prognoses for breaks in the proximal fifth metatarsal, or Jones fracture, that’s known to be slow to heal.
“It wasn’t so much that family medicine practitioners published this orthopaedic project, but that they were residents,” Petrizzi said. “It’s not that easy to do in six years let alone in three. That was the start of Scott’s academic career in my mind. He is a living, breathing example of everything that has come before him. He’s been able to take advantage of his own drive, to learn to the maximum and to have a positive impact on those around him.”
This story was published in the winter 2024-25 issue of 12th & Marshall. You can find the current and past issues online.
Building a legacy
Since its creation, the Department of Family Medicine and Population Health has trained nearly 2,000 physicians. They currently see patients from every ZIP code in the commonwealth. The four years of Strayer’s tenure as chair have seen the department’s footprint grow from two main practice sites to 15, and the new residency program in South Hill is the first new VCU-sponsored training site at VCU Health in more than two decades. The department is ranked 14th nationally among family medicine departments in NIH research funding.
“Our department was founded in 1970 due to projected workforce shortages in primary care,” Strayer said. “Fast forward to today and those shortages are still there but have been stable. I can’t imagine what they would be without the support that we have received from the General Assembly. Our ongoing partnership with the state and support of the school and health system is essential to continue the training that we’re doing to ensure adequate primary care for the commonwealth.
“I go back to the mission of the department,” Strayer said. “To take care of the citizens of Virginia. To provide primary care, yes, but ultimately to take care of them.
“I inherited a wonderful legacy to build on.”
Growing up in Southeast Asia and Latin America, Scott M. Strayer, M’94, H’97, developed a worldview that still guides his life.
“My first memories are being raised in Thailand by people who helped my mom nurture and care for us,” he said. The family moved to Peru and traveled extensively in Latin America and Southeast Asia while overseas. Those multicultural experiences led to his interest in medicine and a desire to take care of people.
“Having an open-minded view of people from various backgrounds has really been incredibly important in my life,” he said. “I’m so thankful that I had that upbringing.”
His father’s job led the family from Peru to Chicago then to Abbott Laboratories in Canada where the elder Strayer worked with infant and adult nutritional products. While that journey exposed young Strayer, as he puts it, “to a little bit of a pharmaceutical and food manufacturing background,” it was a later teenage experience that set the stage for his future in family medicine.
“I like to say that I discovered family medicine twice,” he explained. “Our family physician in Canada would spend every bit of one hour for a visit once or twice a year. Out of that hour, 40 or 50 minutes were spent talking. It was amazing how much he was able to draw out in terms of social history, how we were doing in school, career goals and being able to influence in a gentle way. It was a big part of what really attracted me to family medicine.”
While others may be drawn to the field because of a personal medical experience, Strayer is thankful he had no major medical issues.
“My interest was more in the biopsychosocial model and how you can be a positive influence in a teenager’s world,” he said. “Honestly, I thought, ‘Well, that’s what doctors do.’”
He discovered family medicine the second time as a medical student on the MCV Campus.
“I loved everything about every rotation,” he remembered. “I think that’s a typical family doctor story. And I particularly like procedures. I was leaning toward a surgical specialty or subspecialty, but I started to think about what drew me into medicine and about that early teenage influence of my family physician.”
Today, as the Harris-Mayo Chair of the Department of Family Medicine and Population Health, Strayer draws upon those early experiences to help shape his current role as leader, mentor, counselor and educator for future generations of family practitioners.
A catalyst for improved quality of care
When he learned early in his career that Samuel M. Jones, M’79, former program director of the Fairfax Family Medicine Residency, was credentialed in tympanostomy and tonsillectomies for many years, Strayer was intrigued.
“Sam was still surgically placing ear tubes well into his career as a family physician,” he said. “It gave me the idea that if you were really interested in a particular procedure, you could get that additional training and expertise. And, depending upon where you were practicing – if there’s a need for your expertise – you could do that.”
Obstetrics is another example of the far-reaching benefit of advanced training. While it’s not unusual for family physicians to see OB-GYN patients, many go on to become trained in surgical obstetrics procedures not only because of their procedural interest, but also to improve maternal outcomes, particularly in rural areas where patients may have less access to specialists.
Strayer’s own interests in diagnostic procedures, in fact, led to additional training.
“I actually did a deep dive into endoscopy and became proficient and credentialed,” he said. “I’ve been doing that for 20-plus years and helping to train family docs who then go into underserved areas where there is no one to do an endoscopy. Essentially, we are saving people’s lives by providing access to this critical service for cancer screening.”
When more family physicians are in a geographic area, Strayer said, there’s less maternal and cancer morbidity, and mortality — and improved quality of life.
In July, the department welcomed its inaugural cohort to the VCU Health Community Memorial Hospital residency program in South Hill, Virginia. Near the North Carolina border, the residency program helps attract practitioners to a region with one of the highest rates of colon cancer disparities in the country. “Our new family medicine residency in South Hill is going to be a major catalyst for improving health outcomes in that part of the state,” Strayer said.
A living, breathing example
A prolific researcher (see sidebar), Strayer already has plans to “figure out what’s going on” in the 26 counties east of South Hill with one of the highest colorectal cancer death rates in the country.
In this part of the state, many residents may not be getting screened for colorectal cancer at all. For those that do, a positive stool-blood screening result could mean over an hour’s worth of travel for an endoscopy — a distance that Strayer suspects presents additional barriers for residents, such as taking time off work for further testing and follow-up care.
“If we can find some of the causes and some of the treatment interventions, that’s great,” he said, “but at the end of the day, you need to have folks who can help screen patients to identify the disease early and take care of it before it kills you.”
Strayer is dedicated to ensuring that there are enough physicians to take care of screening and follow up to make up for the lack of access to specialists in the region. The new family medicine residency lays the groundwork to make that promise a reality.
That drive to “figure things out” also served him well in medical school.
In his fourth year, he and a fellow student spent the summer working on an olfactory project led by Richard M. Costanzo, Ph.D., now a professor emeritus in the Department of Physiology and Biophysics.
“We had an interesting finding that there might be some smell distortion with the use of a certain antihypertensive,” Strayer remembered. “We presented it at a regional ear, nose and throat conference. It was my first major medical research presentation.”
After Strayer returned as department chair in 2020, Costanzo, who retired in 2018, ran into him at an event on campus.
“It was exciting to see a former student who had advanced his career to this point,” Costanzo said. “It’s such an asset for medicine to have faculty like Scott who have mastered the art of teaching, research and patient care.”
As a resident, Strayer was the primary author on an orthopaedic research article published in American Family Physician. Under the tutelage of Michael J. Petrizzi, M.D., former director of the VCU Hanover Family Practice Residency, Strayer and fellow resident Steven G. Reece, M’94, H’97, studied treatments and prognoses for breaks in the proximal fifth metatarsal, or Jones fracture, that’s known to be slow to heal.
“It wasn’t so much that family medicine practitioners published this orthopaedic project, but that they were residents,” Petrizzi said. “It’s not that easy to do in six years let alone in three. That was the start of Scott’s academic career in my mind. He is a living, breathing example of everything that has come before him. He’s been able to take advantage of his own drive, to learn to the maximum and to have a positive impact on those around him.”
This story was published in the winter 2024-25 issue of 12th & Marshall. You can find the current and past issues online.
Building a legacy
Since its creation, the Department of Family Medicine and Population Health has trained nearly 2,000 physicians. They currently see patients from every ZIP code in the commonwealth. The four years of Strayer’s tenure as chair have seen the department’s footprint grow from two main practice sites to 15, and the new residency program in South Hill is the first new VCU-sponsored training site at VCU Health in more than two decades. The department is ranked 14th nationally among family medicine departments in NIH research funding.
“Our department was founded in 1970 due to projected workforce shortages in primary care,” Strayer said. “Fast forward to today and those shortages are still there but have been stable. I can’t imagine what they would be without the support that we have received from the General Assembly. Our ongoing partnership with the state and support of the school and health system is essential to continue the training that we’re doing to ensure adequate primary care for the commonwealth.
“I go back to the mission of the department,” Strayer said. “To take care of the citizens of Virginia. To provide primary care, yes, but ultimately to take care of them.
“I inherited a wonderful legacy to build on.”
Improving health outcomes through research
Scott M. Strayer, M’94, H’97, is a national leader in primary care with a focus on health disparities and cancer, working closely with VCU Massey Comprehensive Cancer Center along with his colleagues in family medicine.
In particular, he has significant experience developing innovative approaches to promote behavior change in primary care settings. His current research includes the development of decision aids for lung cancer screening and smoking cessation as well as translational research focused on cancer disparities. Strayer is:
- Co-investigator on a $2.9 million NIH-funded colon cancer disparities grant investigating the role of circadian factors on inflammation and adenoma risk in African Americans;
- Co-founder and past director of the Virginia Practice Support and Research Network, which proved instrumental in involving over 100 Virginia primary care physicians in practice improvement projects using novel health information technology;
- Founder and past president of the American Association of Primary Care Endoscopy;
- Creator of a national registry for smokers that links them to other smokers for social support and to evidence-based social media tools.
Additionally, Strayer has developed NIH-funded computer-assisted tools to enhance smoking cessation, decrease alcohol abuse and misuse, and address poor diet and sedentary lifestyles. He was recently awarded a U.S. patent for a smartwatch that can detect smoking gestures to assist smokers with quitting.
Tags: