Integrating medical science and practice
Our M.D. program is dedicated to the exploration of medicine through dynamic, engaging curriculum that embodies the VCU School of Medicine’s mission of improving health care for humanity.

Curriculum Overview
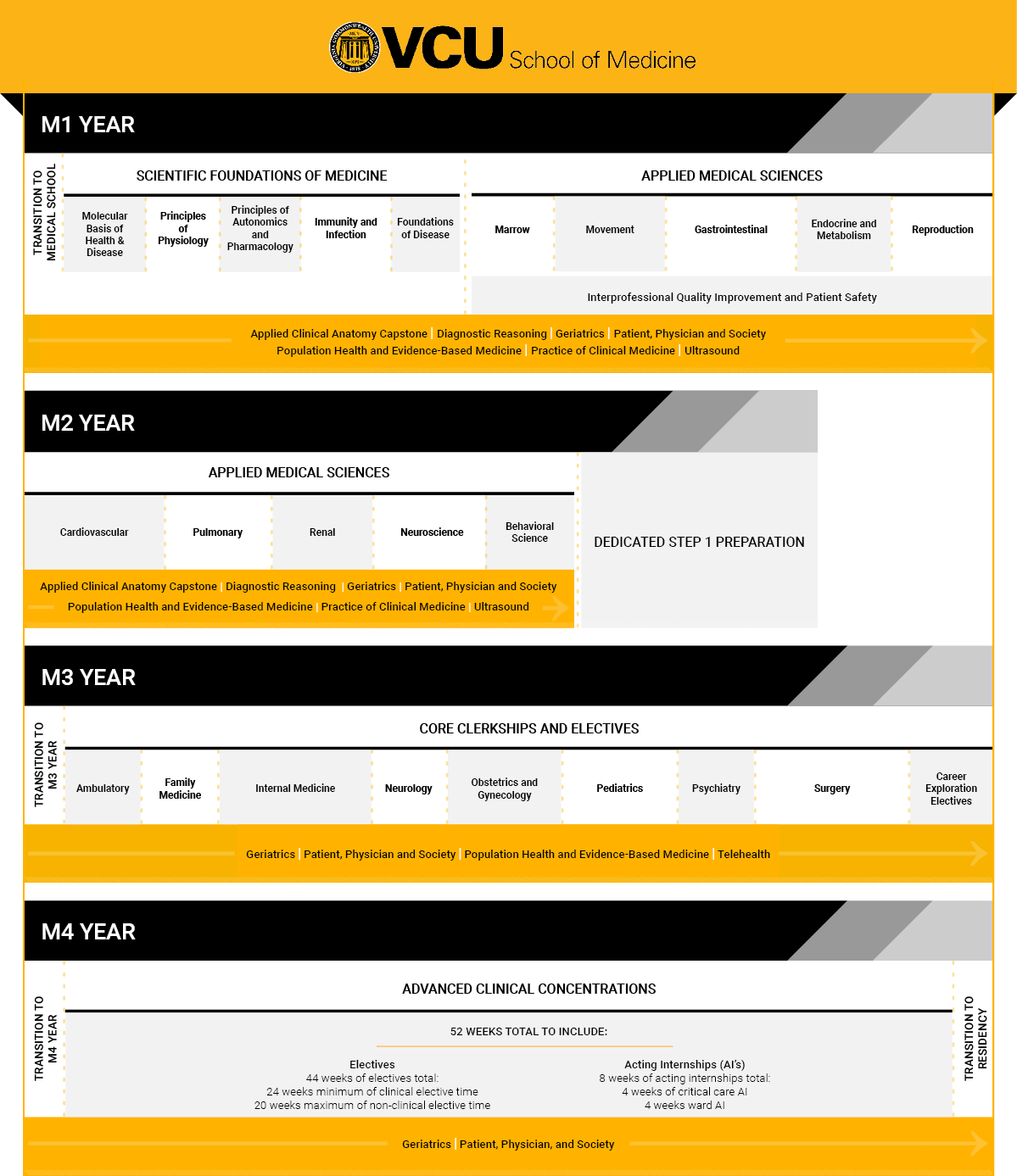
Over the course of four years, students build on foundational knowledge, develop core clinical skills and explore specialty areas under the guidance of some of the top providers in their fields. Longitudinal curriculum throughout the program ensures active learning through the lenses of professionalism, humanism, and compassionate, patient-centered care.

Curriculum at a Glance
M.D. Program Institutional Learning Objectives
Patient Care: The ability to provide patient centered care that is compassionate, appropriate and effective for the treatment of health problems and the promotion of health.
Students who graduate from Virginia Commonwealth University School of Medicine will:
- Obtain and document an organized history and perform a physical examination that is appropriate for the patient’s condition.
- Apply clinical reasoning to develop a differential diagnosis and create an appropriate management plan, including performance of routine procedures after informed consent.
- Select, interpret and understand the indications and limitations of commonly used diagnostic tests, interventions and procedures.
- Apply principles of health equity and the impact of social determinants of health in informing clinical decisions.
- Provide appropriate referral of patients including ensuring continuity of care throughout transitions between providers or settings and following up on patient progress and outcomes.
Knowledge for Practice: The ability to discuss the biomedical, epidemiological and social-behavioral aspects of clinical science and apply this knowledge to patient care.
Students who graduate from Virginia Commonwealth University School of Medicine will:
- Integrate the structure and function of organ systems in health and disease, including the mechanism of therapeutic agents.
- Differentiate the mechanisms by which organ systems are affected by disease and correlate with the epidemiological, clinical, laboratory, radiographic and pathologic manifestations of disease.
- Apply established and emerging principles of evidence-based medicine in the maintenance of health and the diagnosis and treatment of disease.
- Appraise the effect of psychosocial, behavioral and social factors on health and how healthcare disparities and inequities impact communities and populations.
- Explain the underlying ethical principles of research design and the application of the scientific method in basic, clinical and translational research.
Practice-Based Learning & Improvement: Demonstrate the ability to investigate and evaluate one’s care of patients, to appraise and assimilate scientific evidence and to continuously improve patient care based on constant self-evaluation and life-long learning.
Students who graduate from Virginia Commonwealth University School of Medicine will:
- Engage in critical reflection and self-assessment of personal strengths and opportunities for improvement and utilize this information to address gaps in knowledge and improve patient care.
- Contribute to the professional growth of self and team members by soliciting and incorporating feedback and providing formative feedback to others.
- Apply current scientific evidence to optimize clinical care and improve outcomes.
- Utilize available technology to gather data, support care decisions, optimize learning and improve clinical practice.
- Effectively respond to patient needs while balancing personal health and well-being.
Interpersonal & Communication Skills: Demonstrate interpersonal and communication skills that result in the effective exchange of information and collaboration with patients, their families and health professionals.
Students who graduate from Virginia Commonwealth University School of Medicine will:
- Engage in collaborative relationships and work effectively as a member of the health care team across educational, cultural and clinical environments.
- Employ effective communication skills that promote shared decision making with patients and cultivate an inclusive environment that encourages mutual respect for all individuals.
- Communicate compassionately and clearly with patients and their family members to provide education and guidance while respecting individual autonomy.
- Practice effective, efficient, timely communications with members of the healthcare team to maximize patient safety.
Professionalism: Demonstrate a commitment to carrying out professional responsibilities and an adherence to ethical principles while developing one’s professional identity.
Students who graduate from Virginia Commonwealth University School of Medicine will:
- Act responsibly with honesty, integrity, trustworthiness, sensitivity, confidentiality and compassion to create an environment that encourages respect and cultural humility for all.
- Reflect upon and adjust one’s own conscious and unconscious biases when interacting with diverse populations.
- Participate as an active member of the learning community and facilitate lifelong learning of peers and other health care professionals.
- Adhere to the ethical principles pertaining to provision, withholding or withdrawal of care; confidentiality; informed consent; and avoidance of conflicts of interest.
- Demonstrate a commitment to forming one’s own professional identity while executing and adhering to ethical and professional responsibilities of a physician.
Systems-Based Practice: Demonstrate the ability to navigate the healthcare setting and system, identifying and utilizing available resources to provide optimal care for their patients.
Students who graduate from Virginia Commonwealth University School of Medicine will:
- Describe the organization, financing and delivery of healthcare in context of the larger healthcare system.
- Engage in interprofessional collaboration and recognize the role of all members of the healthcare team to optimize patient care.
- Advocate for access to high-value care for patients and appropriate utilization of resources to ensure individuals receive the right care at the right time.
- Identify possible individual and system errors and propose solutions to support patient safety and improve quality of care.
Longitudinal Curriculum
Many M.D. program courses span multiple years, complementing and building upon the scientific, clinical and professional knowledge students gain throughout the four years of medical school.
For more information about our longitudinal curriculum, or to contact a course director, please email the Office of Medical Education: vcuome@vcuhealth.org
The Patient, Physician and Society (PPS) curriculum fosters the development of the humanistic physician during the entire four-year program. The course strives to nurture the caring and compassion for their future patients that students bring with them to school. Topics explored include spirituality, integrative medicine, ethics, cultural competency, palliative care, health care disparities, the impact of psychological trauma on health, the physician-patient relationship, the impact of community and society on individuals’ health, and professionalism.
The Patient, Physician and Society (PPS) curriculum fosters the development of the humanistic physician over the course of all four years, striving to nurture the compassion for their future patients that students bring with them to medical school. Topics explored include:
- Spirituality
- Integrative medicine
- Ethics
- Cultural competency
- Palliative care
- Health care disparities
- The impact of psychological trauma on health
- The physician-patient relationship
- The impact of community and society on individuals’ health
- Professionalism
The Practice of Clinical Medicine (PCM) course, which occurs over the first 18 months, covers basic clinical skills such as professionalism, medical interviewing, physical examination and clinical reasoning. These skills are practiced in a small group setting and taught by a practicing attending physician and a volunteer M4 student. During M2, students have the chance to put their new knowledge to use by interacting with patients alongside a preceptor either at VCU or in the community two afternoons a month.
The Interprofessional Education and Collaborative Care (IPEC) curriculum includes required courses during M1 and M4, plus electives available during M2 and M3. Courses include:
- Foundations of Interprofessional Practice
- Interprofessional Quality Improvement and Patient Safety
- Interprofessional Communication and the Care Coordinator
- Health Care and Care Coordination
- Health Care Payment Models and Care Coordination
- Ethical and Legal Considerations in Care Coordination
- Mindfulness Practices for Health Care Professionals: Clinical Applications
- Global Health
- Interprofessional Complex Care Coordination
- Interprofessional Special Topics
The Population Health and Evidence-Based Medicine course teaches epidemiology, biostatistics, preventive medicine, public health and evidence-based medicine throughout the first three years.
A longitudinal course that runs through the first 18 months of the preclinical curriculum, Point of Care Ultrasound gives students the chance to learn bedside clinical ultrasound while they learn basic physical exam and history skills during their Practice of Clinical Medicine course. Each session has a standardized patient to scan, and pathologies will be discussed or displayed on the simulators.
Diagnostic Reasoning (DR) is an 18-month longitudinal course that has two distinct but related purposes:
- Prepare for M3 by honing critical thinking and diagnostic skills and building differential diagnosis capabilities.
- Prepare for the Step 1 examination through the use of USMLE-style multiple choice questions.
Developed using the core competencies as defined by the American Geriatrics Society and the Association of American Medical Colleges, this four-year curriculum includes interactive case-based sessions, patient and caregiver panels and online case simulation. By the end of M4, students will be able to evaluate older patients that exhibit acute and chronic illness in a manner consistent with the patients’ prognosis, values and goals. The management of older patients will be informed by a core-defined knowledge of age-related changes in human biology and pharmacology, as well as systems of care.
Students also learn how to manage common geriatric syndromes and conditions, including (but not limited to):
- Delirium
- Dementia
- Immobility
- Falls
- Under-nutrition
- Polypharmacy
- Pre- and post-operative complications
- Social isolation
- Failure to thrive
- Discharge planning
- Elder abuse
This longitudinal exercise, from January of M1 to January of M2, incorporates anatomical, radiological, pathological and other clinical observations into an integrated assessment of a cadaver’s anatomy and suspected medical problems. To enhance this cumulative, longitudinal exercise, students can excise suspected pathological tissues and submit them to the Department of Pathology. Daily logs of anatomical observations and findings with potential clinical relevance aid with documentation and tabulation of information, especially when multiple casualty-related symptoms are present. The final presentation is a self-directed group exercise in which each dissection table formally presents their dissection findings that identifies at least one significant clinical condition (not necessarily the cause of death) that the patient experienced when they were alive. This presentation is in a Grand Rounds style, presented to fellow students and faculty and judged and scored by a team of anatomy and clinical faculty.
Special Programs
Year-Out Program for Biomedical Research
Acute Care and System Strengthening (ACCESS) in Low-Resource Settings
International/Inner City/Rural Preceptorship (I2CRP)
Family Medicine Scholars Training and Admission Track (fmSTAT)